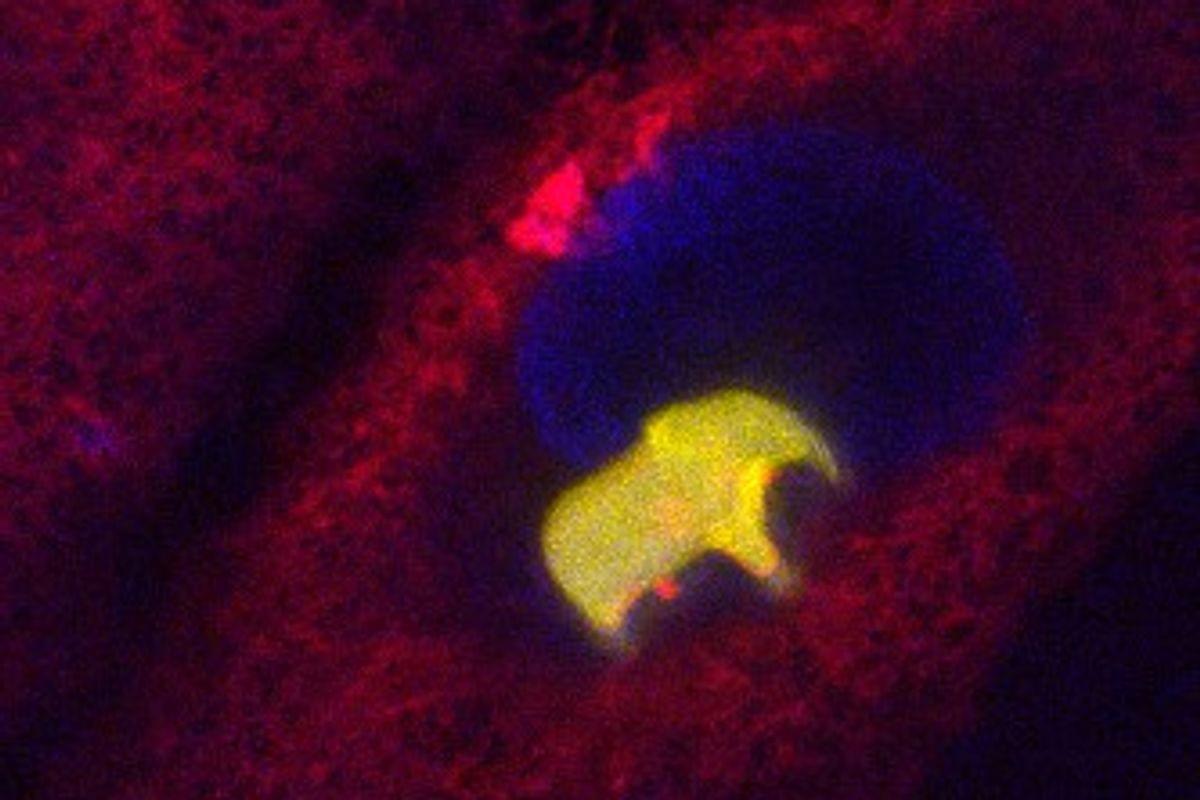
Multiphoton microscopy is used in biomedical research to study cells and tissues. Today, so-called two-photon microscopy is used to study processes within cells, but the technique has limitations in terms of image resolution. Four-photon microscopy provides images with higher resolution. However, such instruments are very expensive and, when studying biological material, the powerful laser light required can damage samples.
“In this project, we have developed molecules to visualize molecular-level details and monitor processes using the more common two-photon microscopy technique. These molecules have the capacity to achieve higher resolution than with four-photon microscopy, although two-photon microscopy is used,” says the project coordinator Joakim Andréasson, Professor at the Department of Chemistry and Chemical Engineering at Chalmers University of Technology.
“In the long term, results from studies of this kind may provide new insights into diseases, pharmaceuticals and the very smallest building blocks of life.”