A paper describing Hopp’s upcoming study published on the CureAlz website, titled, “How Do Microglia Contribute to the Spread of Tau Pathology in Alzheimer’s Disease?”, says that while tau aggregates are a defining feature of Alzheimer’s disease and closely track with brain cell loss, memory problems and cognitive decline, much still isn’t known about how it spreads or what role the brain’s immune system plays in the process.
There is evidence, it says, that toxic forms of tau, which have become “misfolded” or dysfunctional, act like a “bad influence.”
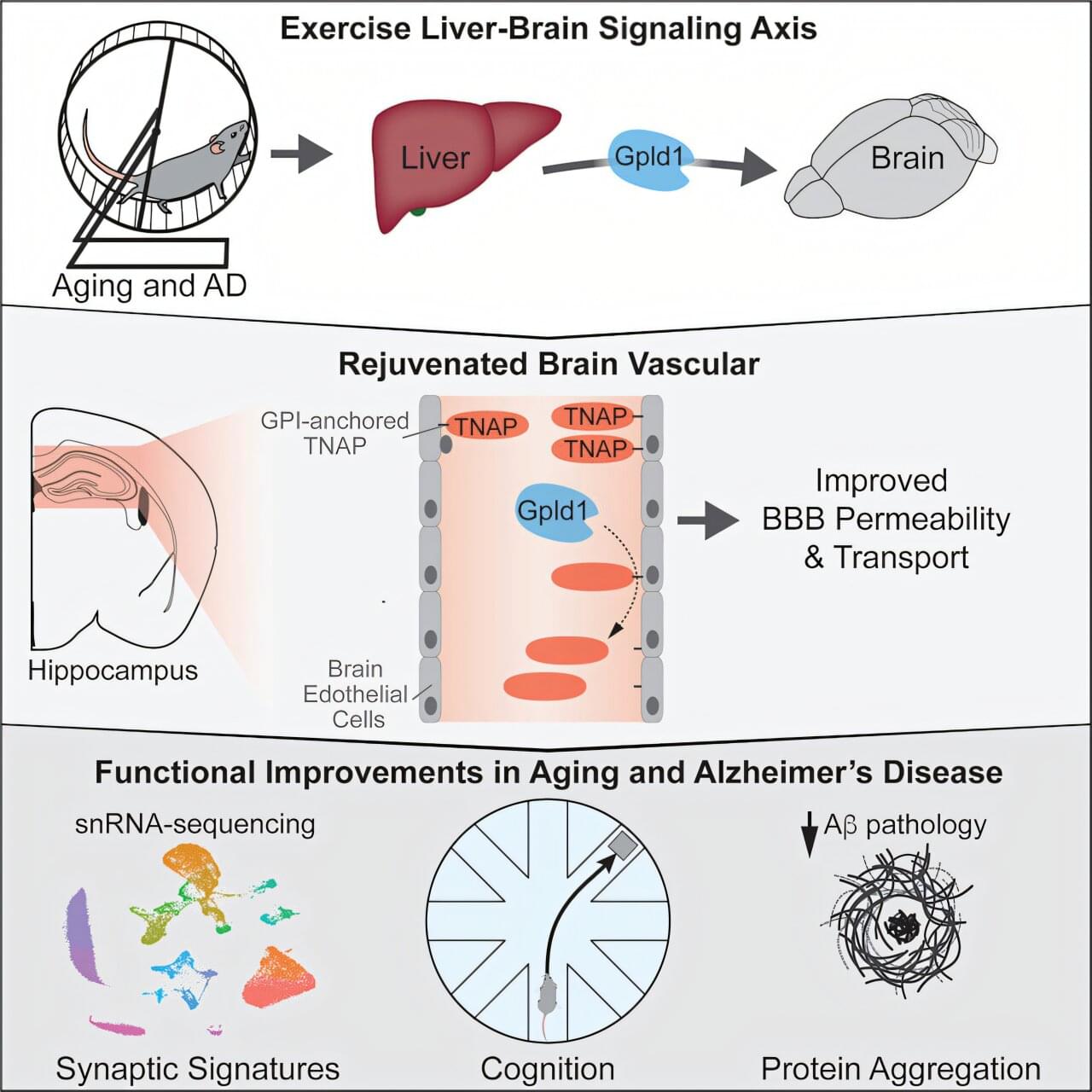
“When they encounter nearby healthy tau proteins, they cause them to misfold as well, triggering a chain reaction that spreads from one brain region to another,” according to the paper. “Microglia … are among the first to encounter these toxic tau ‘seeds.’ Normally, microglia protect the brain by clearing debris and helping repair damage. But growing evidence suggests that microglia may also contribute to tau’s spread by engulfing misfolded tau and inadvertently releasing it, thereby amplifying its harmful effects.”
A researcher with the Glenn Biggs Institute for Alzheimer’s and Neurodegenerative Diseases at UT Health San Antonio has received a two-year, $402,500 grant award from the Cure Alzheimer’s Fund to study how microglia, the brain’s resident immune cells, paradoxically might contribute to the spread of toxic forms of tau protein in the disease.
Sarah C. Hopp, PhD, associate professor of pharmacology with the Biggs Institute and the South Texas Alzheimer’s Disease Research Center, along with her lab have been instrumental in uncovering the behavior of microglia. UT Health San Antonio is the academic health center of The University of Texas at San Antonio.
Starting this month, Hopp’s lab will test the hypothesis that microglial uptake of tau is a key mechanism driving its spread through the brain, and that specific molecular pathways determine whether this process protects or harms neurons. The Cure Alzheimer’s Fund, also known as CureAlz, is a nonprofit organization that funds research “with the highest probability of preventing, slowing or reversing Alzheimer’s disease.”