The new study, published in the journal Nature, provides new insights by demonstrating that while different mutations affect the developing brain in initially distinct ways, they increasingly impact overlapping molecular pathways as development progresses.
Researchers monitored the gene expression of the organoids over 100 days as they developed, which allowed researchers to observe how genetic changes affect brain during the critical early development windows.
Early in development, each genetic form showed distinct molecular signatures. However, as the organoids matured, these different mutations increasingly affected similar biological processes, particularly those involved in neuronal maturation and synapse formation.
The researchers identified a network of genes involved in regulating gene expression and chromatin remodeling, which is the process by which DNA is packaged and made accessible for reading. This network appears to play a central role in this convergence. Using CRISPR technology to individually reduce the activity of these regulatory genes in neural cells, the team confirmed that many of them control downstream pathways were previously linked to autism.
Notably, the study found few consistent molecular changes in organoids derived from individuals with idiopathic autism, likely reflecting the highly complex genetic architecture of autism that doesn’t involve major mutations. This finding underscores the need for much larger studies to understand the more common, polygenic forms of autism. ScienceMission sciencenewshighlights.
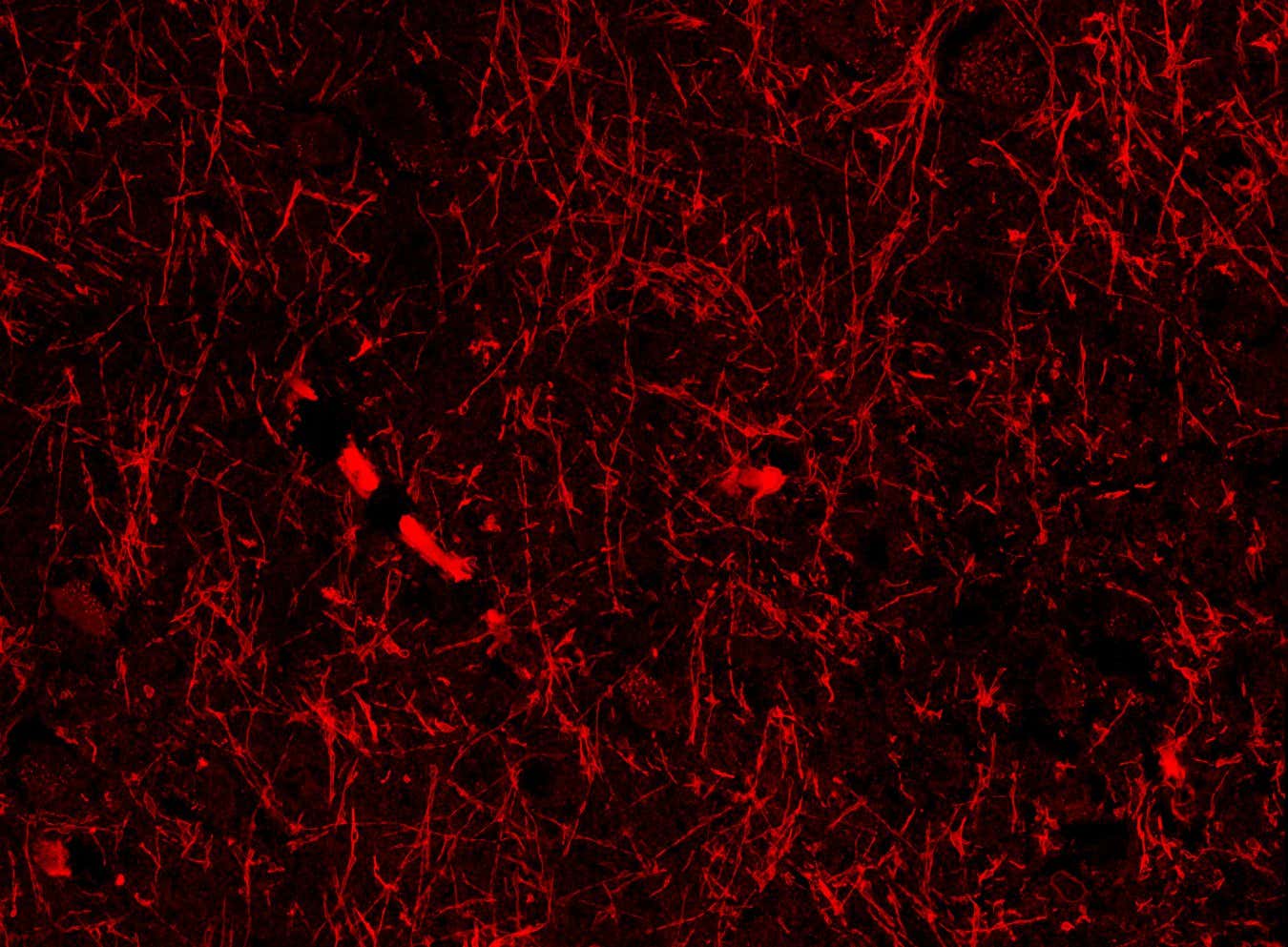
The researchers have created a comprehensive map showing how eight different genetic mutations associated with autism spectrum disorder affect early brain development, providing new insights into the ways diverse genetic causes may lead to shared features and symptoms of the disorder.