The innovative material that creates green energy through mechanical force.
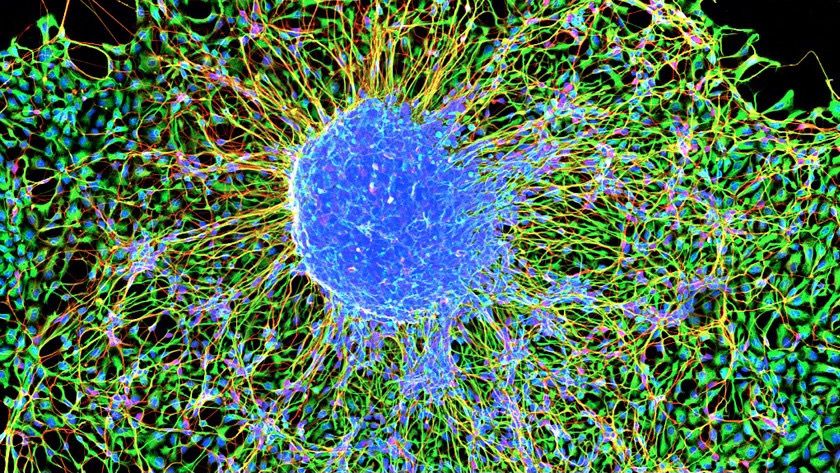
A new nanotechnology development by an international research team led by Tel Aviv University researchers will make it possible to generate electric currents and voltage within the human body through the activation of various organs (mechanical force). The researchers explain that the development involves a new and very strong biological material, similar to collagen, which is non-toxic and causes no harm to the body’s tissues. The researchers believe that this new nanotechnology has many potential applications in medicine, including harvesting clean energy to operate devices implanted in the body (such as pacemakers) through the body’s natural movements, eliminating the need for batteries.
The study was led by Prof. Ehud Gazit of the Shmunis School of Biomedicine and Cancer Research at the Wise Faculty of Life Sciences, the Department of Materials Science and Engineering at the Fleischman Faculty of Engineering, and the Center for Nanoscience and Nanotechnology, along with his lab team, Dr. Santu Bera and Dr. Wei Ji.