Category: bioengineering – Page 162
New CRISPR-based system targets amplified antibiotic-resistant genes
Taking advantage of powerful advances in CRISPR gene editing, scientists at the University of California San Diego have set their sights on one of society’s most formidable threats to human health.
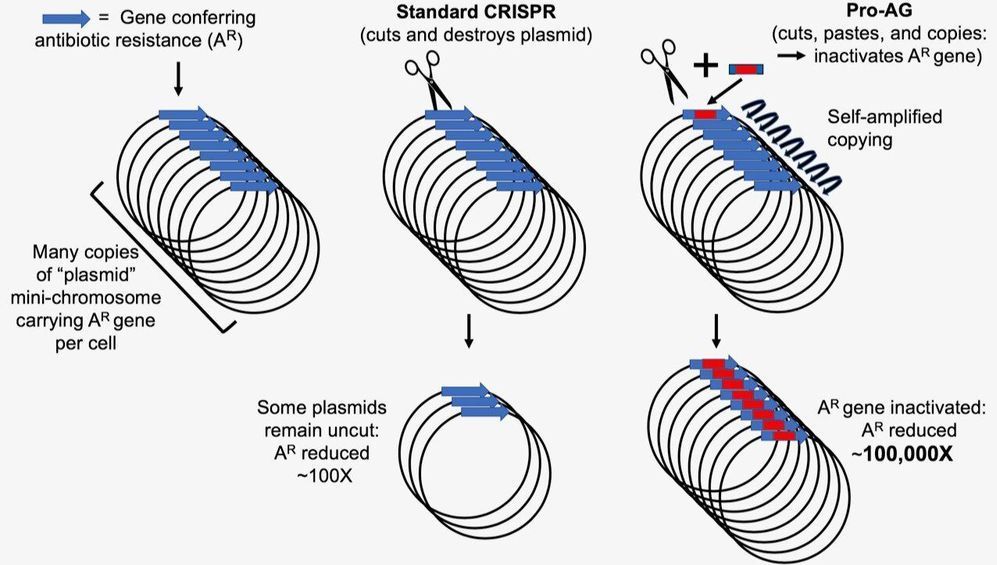
A research team led by Andrés Valderrama at UC San Diego School of Medicine and Surashree Kulkarni of the Division of Biological Sciences has developed a new CRISPR-based gene-drive system that dramatically increases the efficiency of inactivating a gene rendering bacteria antibiotic-resistant. The new system leverages technology developed by UC San Diego biologists in insects and mammals that biases genetic inheritance of preferred traits called “active genetics.” The new “pro-active” genetic system, or Pro-AG, is detailed in a paper published December 16 in Nature Communications.
Widespread prescriptions of antibiotics and use in animal food production have led to a rising prevalence of antimicrobial resistance in the environment. Evidence indicates that these environmental sources of antibiotic resistance are transmitted to humans and contribute to the current health crisis associated with the dramatic rise in drug-resistant microbes. Health experts predict that threats from antibiotic resistance could drastically increase in the coming decades, leading to some 10 million drug-resistant disease deaths per year by 2050 if left unchecked.
Nanoscience breakthrough: Probing particles smaller than a billionth of a meter
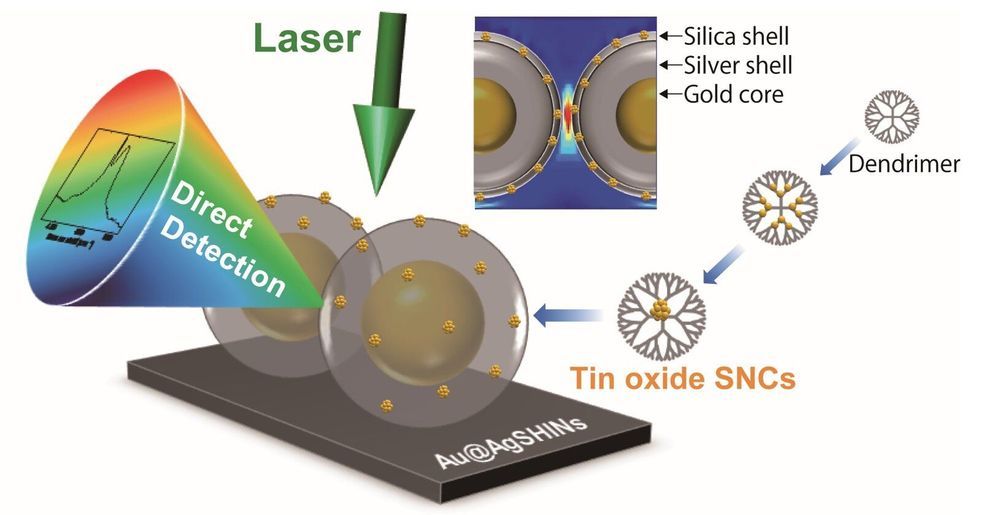
Scientists at Tokyo Institute of Technology (Tokyo Tech) have developed a new methodology that allows researchers to assess the chemical composition and structure of metallic particles with a diameter of only 0.5 to 2 nm. This breakthrough in analytical techniques will enable the development and application of minuscule materials in the fields of electronics, biomedicine, chemistry, and more.
The study and development of novel materials have enabled countless technological breakthroughs and are essential across most fields of science, from medicine and bioengineering to cutting-edge electronics. The rational design and analysis of innovative materials at nanoscopic scales allows us to push through the limits of previous devices and methodologies to reach unprecedented levels of efficiency and new capabilities. Such is the case for metal nanoparticles, which are currently in the spotlight of modern research because of their myriad potential applications. A recently developed synthesis method using dendrimer molecules as a template allows researchers to create metallic nanocrystals with diameters of 0.5 to 2 nm (billionths of a meter).

Viewpoint: Rampage movie offers twisted take on CRISPR gene editing
Is a film based on a video game with fleeting mentions of a biotech buzzword compelling sci-fi? No. But I liked Rampage anyway.
The use of CRISPR to edit genes is perhaps the only novel plot point in this latest monster movie. An evil head of a biotech company subverts a scientist’s work to fashion a bioweapon that revs up the growth hormone gene, and more, in three unfortunate animals. Cue Godzilla, King Kong, and the beast in Lake Placid.
But the screenwriters seem to confuse gene editing with an infectious bioweapon, like anthrax. The tagline at IMDb reveals the befuddlement: “When three different animals become infected with a dangerous pathogen, a primatologist and a geneticist team up to stop them from destroying Chicago.” Infectious disease, genetic modification, or both?

CRISPR Human Trial Results Look Promising for Safety
Recently, the first attempt in the United States to use the gene editing tool CRISPR to combat cancer appears to have gone well, according to the initial results of a small human trial to determine safety for the approach.
Gene editing is a way to permanently change DNA in order to potentially cure a disease by attacking the root causes. CRISPR is a tool that can cut DNA at a specific spot, allowing genes to be removed or replaced or new genes to be inserted. CRISPR and other similar gene editing tools have long been used in the lab and are finally, after many years, starting to reach human trials for cancer and other diseases.
The approach involved doctors harvesting immune T cells from three cancer patients’ bloodstreams and modifying those cells with CRISPR to make them better able to detect and destroy cancer. Two of the patients have multiple myeloma, and the third has a sarcoma. Essentially, this therapy uses the body’s own immune cells to fight the disease rather than going with the traditional route of using drugs to disrupt the growth and spread of cancer.

A Step Closer to a Bioengineered Liver Fit for Transplantation
Currently over 6,300 people in the UK are waiting for an organ transplant, and sadly everyday around three people die waiting. In efforts to reduce the reliance on organ donors and improve the outlook for patients, alternative sources of organs are being explored by several research groups.
In a study recently published in Nature Biomedical Engineering, bioengineered livers created by decellularization and recellularization were implanted into pigs, where they were able to sustain continuous perfusion for up to 15 days. We spoke to Miromatrix’s CEO, Dr Jeff Ross, to learn more about the study and how it advances the state of bioengineering organs.
Anna MacDonald (AM): What are some of the main challenges faced when creating bioengineered organs?

How 3D-printing robots will get Mars home-ready for our arrival
NASA has tentative plans for a manned mission to Mars sometime in the 2030s. Between now and then, there’s still much that needs to be sorted. To start, massive dust storms, high levels of radiation, low temperatures and a lack of water make the Martian surface an unfriendly place for long-term visits. Taming it for human life will likely prove one of the most demanding and complex engineering puzzles in human history. With those extraordinary obstacles in mind, in 2015 NASA announced the 3D-Printed Habitat Challenge: an open call asking designers and architects outside the traditional aerospace industry to create plans for Martian living centred around 3D printing. One of 10 finalists announced in 2019, this plan from the design practices HASSELL and Eckersley O’Callaghan envisions teams of 3D-printing robots building a protective shield on the Martian surface several months in advance of a human landing. Upon arrival, astronauts would then work alongside the autonomous robots to piece together an inflatable, modular habitat.
Video by LightField London.

Transhumanism and Immortality
I am in shock… Google suddenly as yahoo are allowing conjecture and mendacity be seen as public or scientific opinion. Here is another confused mind who towards the end of her rant quotes Christian scripture as basis to stop Life extension-Transhumanism???
When I say to these minds Behold the leader of Christianity stood for Life abundant-Super Longevity and I can prove such. No matter what lost evangelist or preacher tells you Jesus was a medical researcher of extraordinary magnitude…
NOW BEHOLD THE LOST in this article… https://www.rodofironministries.com/…/transhumanism-and-imm… Respect r.p.berry & AEWR wherein aging now ends we have found the many causes of aging and we have located an expensive cure. We search for partners-investors to now join us in agings end… gerevivify.blogspot.com/
Whether we like it or not, the hybrid age is already here. From genetic manipulation, to AI technology, to nano-technology, robotics, 3D printing, brain mapping, super computing, the list is literally endless. Futurists and Transhumanist philosophers believe that science and technology are limitless, and that humanity’s current cultural traditions and mindset are the mechanisms in place that prohibit human development.
Mankind has experienced formidable technological growth in the past from the early ancestors to the Agrarian Age, the Industrial Age in the 18th century, and the Information Age in the 1970s, from their point of view, we are simply going through another revolutionary leap into what they call, the Hybrid Age.
The Transhumanist Movement, also known as H+ is an intellectual, cultural and political movement that supports technological enhancements in the human body through the use of genetics, robotics, synthetic biology, AI technology among others to modify the physiology, psyche, memory and progeny of a human being and ultimately achieve immortality on earth, (a procedure they believe can be reached within the next decade) whereby human consciousness can be uploaded into a robot, cyborg or possibly, a human clone. The sci-fi novel “Altered Carbon” by Richard K. Morgan captures a cornucopia of technological concepts that are, believe it or not, in experimental stages across the globe, methods such as: human hybridization, CRISPR-technology—Chinese scientists have used CRISPR for gene-editing on 86 human patients; limb regeneration, bionic augmentation, the making of super-soldiers, cloning, Cryonics and the growing interest in information-theoretic death, neuropreservation, suspended animation, molecular nano-technology and so on. Sounds far-fetched right?