Advanced psc-based strategies for leukodystrophy therapy👇
✅Pluripotent stem cell (PSC)–based technologies are opening new avenues for the treatment of leukodystrophies by combining cell replacement, gene correction, disease modeling, and drug discovery within a unified framework.
✅One major approach focuses on the development of off-the-shelf PSC-derived neural progenitor cells (NPCs). By precisely editing immune-related genes, PSCs can be engineered to evade immune rejection. Strategies include knocking out core components of HLA class I and II pathways while introducing protective molecules such as HLA-E, or selectively removing highly immunogenic HLA alleles. These modifications allow the generation of universal donor NPCs that are resistant to T cell– and NK cell–mediated killing.
✅Autologous induced pluripotent stem cell (iPSC) therapy represents a personalized treatment strategy. Patient-derived somatic cells are reprogrammed into iPSCs, followed by genetic correction of disease-causing mutations using viral vectors or CRISPR/Cas9-based editing. Corrected iPSCs are then differentiated into neural stem cells (NSCs), NPCs, or oligodendrocyte progenitor cells (OPCs) and transplanted back into the same patient, minimizing immune complications.
✅Beyond therapy, iPSC-based disease models provide powerful tools to study leukodystrophy pathogenesis. Disease-specific iPSCs recapitulate key cellular phenotypes such as impaired differentiation, lysosomal dysfunction, oxidative stress, and apoptosis. These models enable direct investigation of early developmental defects that are difficult to access in patients.
✅Corrected iPSCs restore normal cellular phenotypes, allowing direct comparison between diseased and healthy isogenic cells. This approach clarifies causal mechanisms and validates gene correction strategies at the cellular level, supporting precision medicine.
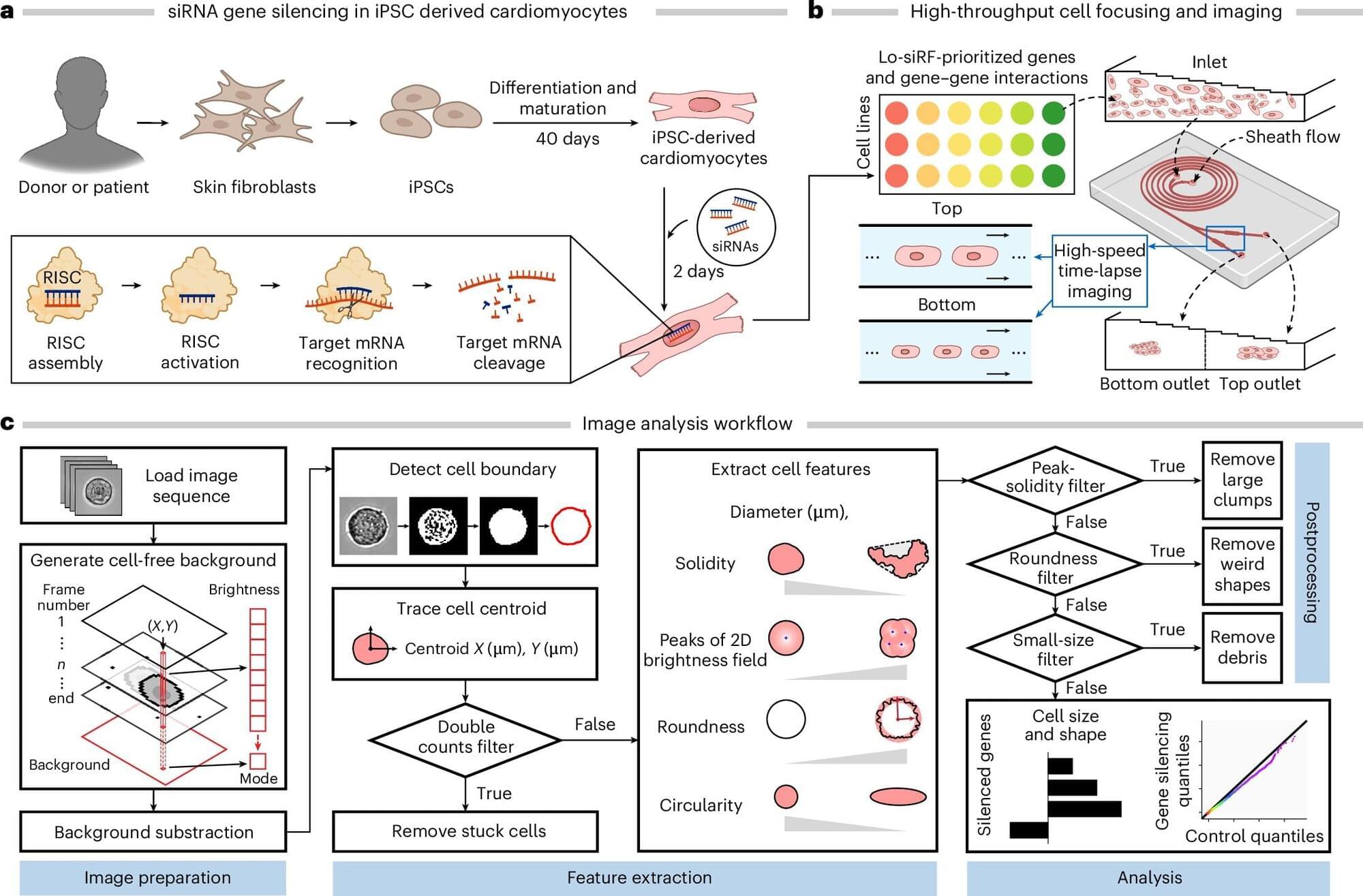
✅iPSC-derived neural systems also support advanced drug discovery platforms. By generating complex neural cultures or myelinating organoids (“myelinoids”), researchers can model neuron–glia interactions and myelination in vitro. Coupled with immunofluorescence, transcriptomics, and high-throughput screening, these systems enable systematic identification of small molecules that promote myelination or correct metabolic defects.