Complement inhibition showed promising clinical improvement in this single case of dysferlinopathy.
Dysferlinopathy is a rare autosomal recessively inherited myopathy, presenting as several phenotypes, including a proximal weakness dominant limb-girdle muscular dystrophy R2 phenotype and a distal weakness dominant Miyoshi distal myopathy phenotype.1,2 Muscle weakness usually emerges in young adulthood, followed by a progressive motor decline over the first decade, which tends to be more rapid in individuals with earlier onset.3 Dysferlinopathy is caused by pathogenic variants of the DYSF gene that impair function of dysferlin, a protein that cooperates with others to repair membranes and restore skeletal muscle integrity after injury.4
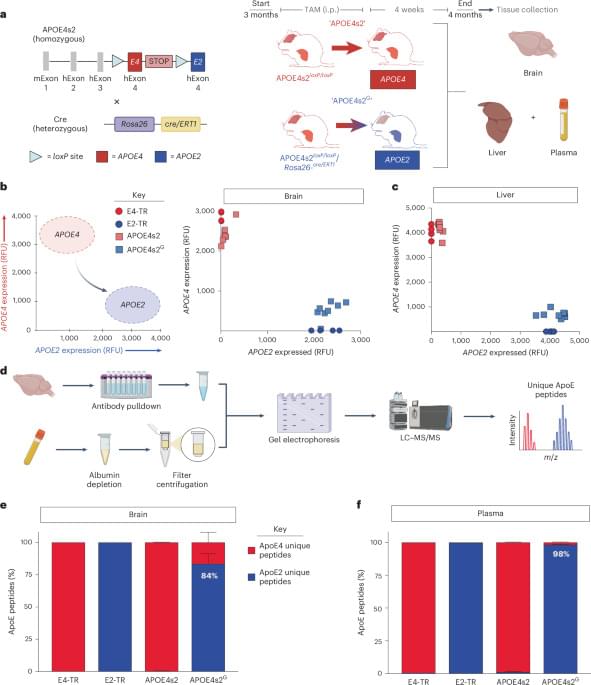
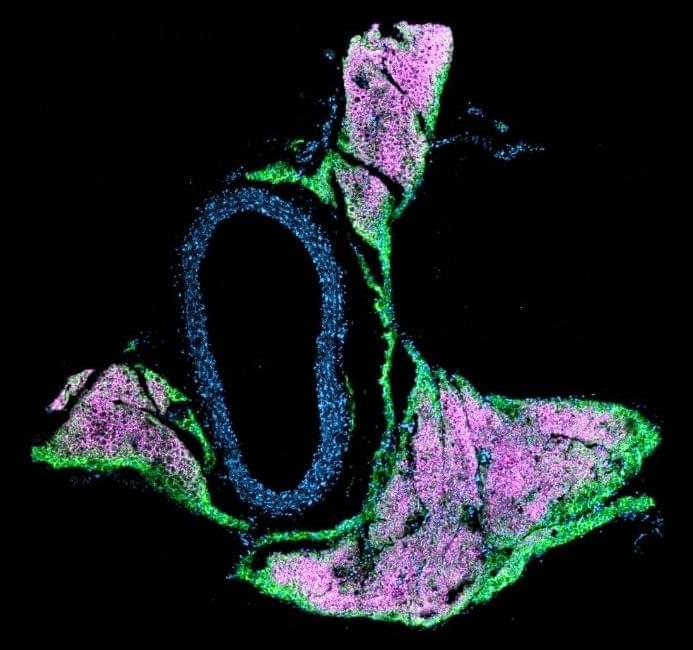
To date, no effective treatment for dysferlinopathy has been clinically validated. Promising approaches, including exon skipping and gene editing targeting the DYSF gene, as well as myoblast transplantation, are still under investigation in preclinical models.5 Although dysferlinopathy often presents with inflammatory features on muscle pathology and is prone to misdiagnosis as myositis, it is characterized by the absence of focal MHC-I expression and complement C5b-9 deposition on nonnecrotic sarcolemma, which help distinguish it from other muscular dystrophies and inflammatory myopathies.6,7 Specially, complement C3 gene knockout in dysferlin-deficient mice has been demonstrated being able to reverse muscle pathology and improve motor function in the previous animal research.