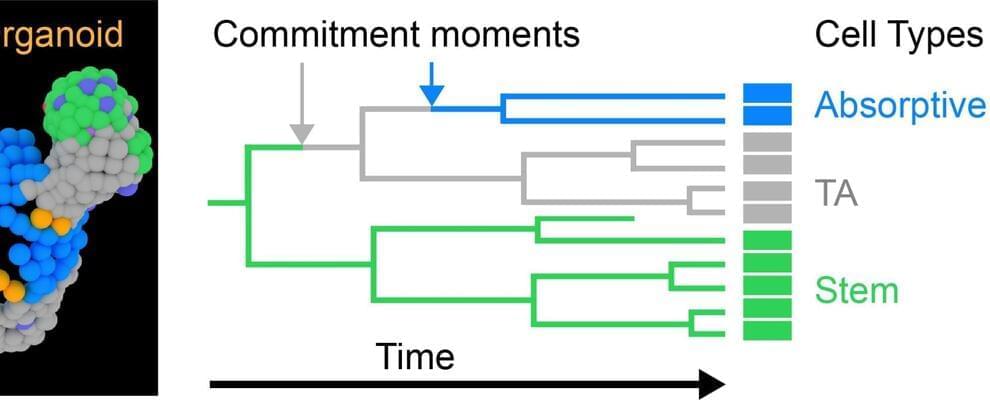
AMOLF researchers discovered that stem cells first specialize into a functional cell and then move to their proper location—rather than the other way around.
Researchers at AMOLF, Amsterdam, and the Hubrecht institute, Utrecht, revealed a new model to show how stem cells specialize into functional cells. They found that their position in the organ is not as important as current models claim. Rather, stem cells choose their identity first and only then move to their appropriate position.
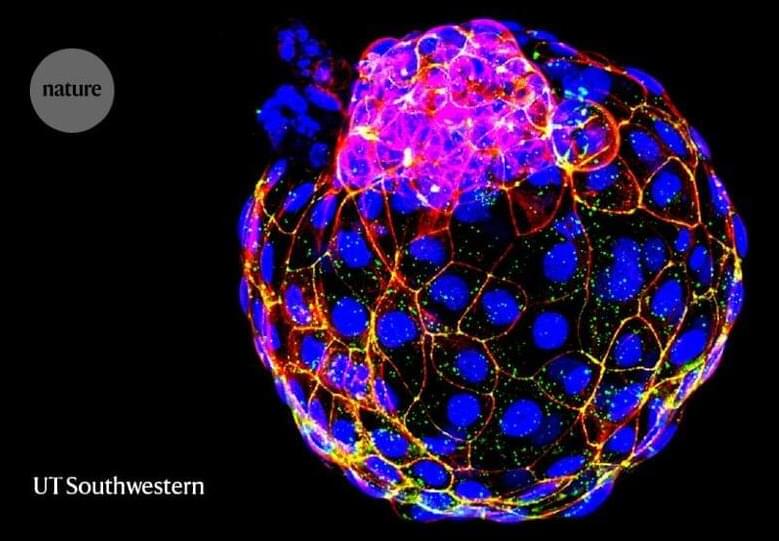
These discoveries were made using intestinal organoids and the new TypeTracker technique, which can now be used to understand other organs at the cellular level and the effects of mutations and medications. The findings were published on August 18 in the journal Science Advances.