Prochlorococcus is the smallest and numerically most abundant cyanobacterium in the oceans. It has a large pangenome and hypervariable genomic islands linked to niche differentiation and phage defense. The smallest and most numerous cyanobacterium in the oceans is Prochlorococcus.
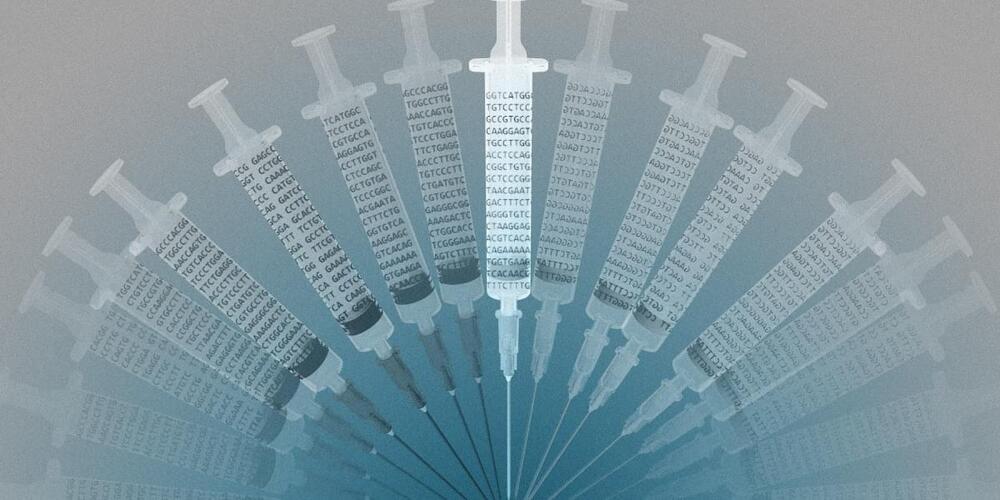
According to recent research by MIT, these microscopic bacteria communicate with one another by a previously unidentified mechanism, even when they are far apart. Because of this, they can pass along entire gene sets, such as those enabling them to assimilate a certain type of nutrition or protect themselves against viruses, even in areas where their population in the water is quite low.
According to the findings, a new class of genetic agents involved in horizontal gene transfer —in which genetic material is directly transferred across animals, whether they are of the same species or not—has been discovered by methods other than lineal descent. Tycheposons are DNA sequences that can spontaneously detach from surrounding DNA and can include multiple complete genes, according to scientists.