Join us as we meet the engineers, entrepreneurs, doctors and patients who are giving people a new lease on life today, while building our future of tomorrow.


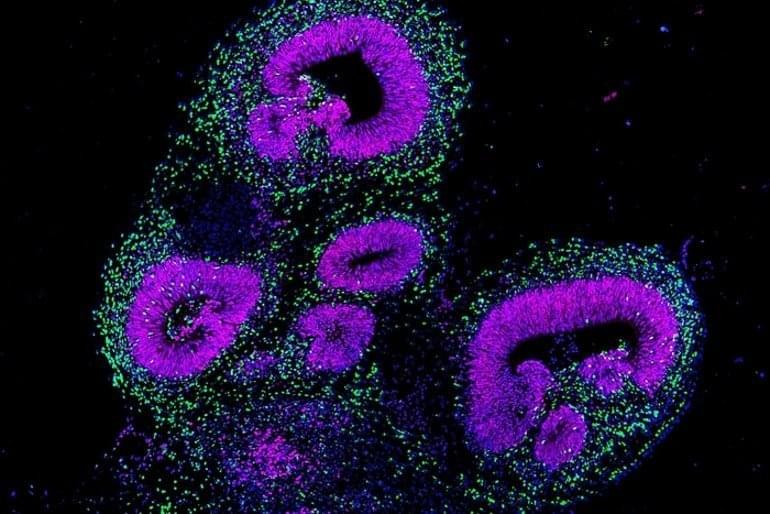
Summary: Brain organoids are helping researchers map the molecular, genetic, and structural changes that occur during brain development.
Source: ETH Zurich.
The human brain is probably the most complex organ in the entire living world and has long been an object of fascination for researchers. However, studying the brain, and especially the genes and molecular switches that regulate and direct its development, is no easy task.

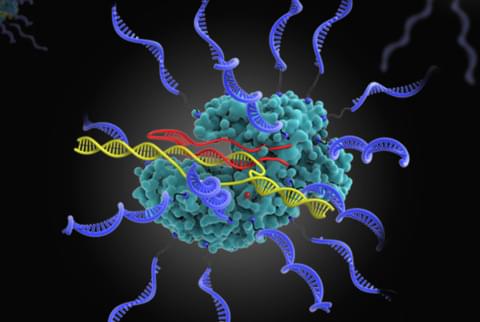
A team of researchers at Northwestern University has devised a new platform for gene editing that could inform the future application of a near-limitless library of CRISPR-based therapeutics.
Using chemical design and synthesis, the team brought together the Nobel-prize winning technology with therapeutic technology born in their own lab to overcome a critical limitation of CRISPR. Specifically, the groundbreaking work provides a system to deliver the cargo required for generating the gene editing machine known as CRISPR-Cas9. The team developed a way to transform the Cas-9 protein into a spherical nucleic acid (SNA) and load it with critical components as required to access a broad range of tissue and cell types, as well as the intracellular compartments required for gene editing.
The research, published today in a paper titled, “CRISPR Spherical Nucleic Acids,” in the publication Journal of the American Chemical Society, and shows how CRISPR SNAs can be delivered across the cell membrane and into the nucleus while also retaining bioactivity and gene editing capabilities.
Today there might not be a cure to save your life. What if the cure were available tomorrow? Biostasis (cryonics) is a possibility for keeping you around long enough for the cure.
NIH researchers reveal new insights on how genetic architecture determines gene expression, tissue-specific function, and disease phenotype in blinding diseases.
National Eye Institute (NEI) scientists have mapped the organization of human retinal cell chromatin. These are the fibers that package 3 billion nucleotide-long DNA
DNA, or deoxyribonucleic acid, is a molecule composed of two long strands of nucleotides that coil around each other to form a double helix. It is the hereditary material in humans and almost all other organisms that carries genetic instructions for development, functioning, growth, and reproduction. Nearly every cell in a person’s body has the same DNA. Most DNA is located in the cell nucleus (where it is called nuclear DNA), but a small amount of DNA can also be found in the mitochondria (where it is called mitochondrial DNA or mtDNA).
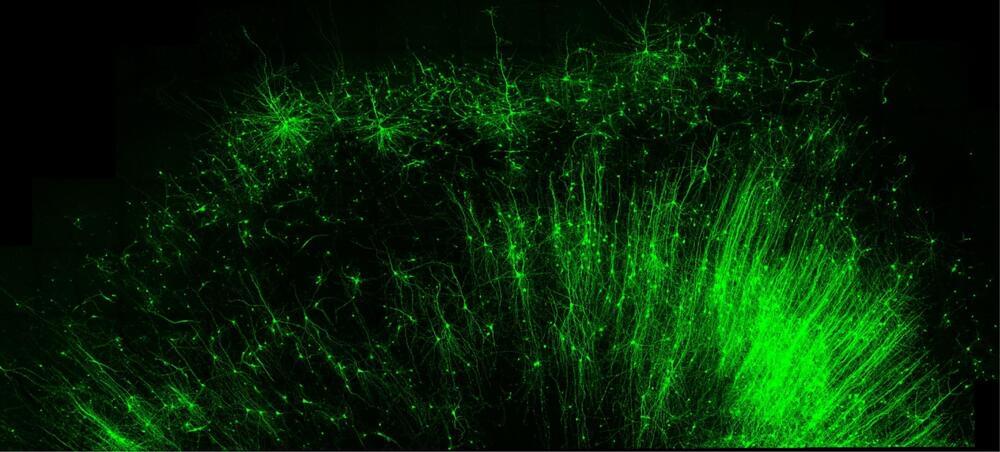
Editing technology is precise and broadly applicable to all tissues and species.
Scientists at Duke University have developed an RNA
Ribonucleic acid (RNA) is a polymeric molecule similar to DNA that is essential in various biological roles in coding, decoding, regulation and expression of genes. Both are nucleic acids, but unlike DNA, RNA is single-stranded. An RNA strand has a backbone made of alternating sugar (ribose) and phosphate groups. Attached to each sugar is one of four bases—adenine (A), uracil (U), cytosine ©, or guanine (G). Different types of RNA exist in the cell: messenger RNA (mRNA), ribosomal RNA (rRNA), and transfer RNA (tRNA).
No one imaging mode can catch everything that’s going on inside the brain, since it is such a complex organ. Multiple “brain maps” have emerged over the years, with each focusing on different brain processes, from metabolism to cognitive function. These maps are indeed important, but using them in isolation limits the discoveries scientists can make from them.
More than forty existing brain maps have now been collected in one place by a team from The Neuro. Called neuromaps, the database will help researchers find correlations between patterns across different brain regions, modalities, spatial scales, and brain functions. To assist researchers in differentiating between a relevant association and a random pattern, it offers a standardized space to see each map in comparison to one another and evaluates the statistical significance of these comparisons. Additionally, the neuromaps database helps standardize the code across maps, to improve reproducibility of results.

One of the hallmarks of aging, cellular senescence is what happens when aging cells do not die in the usual way (a process known as apoptosis) and start to accumulate in our bodies. The accumulation of these “senescent” cells is implicated in diseases including dementias, atherosclerosis, cancers, diabetes and arthritis. But senescence is not just part of the aging process – it tends to occur in individuals who develop frailty and multiple illnesses, and this can occur at any point during life.
In 2015, a team of researchers at the Mayo Clinic, led by Dr James L Kirkland, published a seminal paper in Aging Cell that introduced a new class of drugs called senolytics. Based on the idea that removing senescent cells may enhance human healthspan, these drugs were identified based on their ability to selectively target and eliminate those cells.
Longevity. Technology: Since the discovery of the first senolytics, hundreds of others have since been identified or created, and senotherapeutics is now one of the hottest areas in longevity, with a host of clinical trials under way and companies pursuing senolytic therapies for a range of age-related conditions. But what does the man who started it all think about the therapeutic field he helped create? In the first of two articles, we bring you Dr Kirkland’s unique perspective on the world of senolytics.

Scientists have discovered what turns off the molecular alarm system that plays a critical role in our immune response.
The antibacterial superhero MR1 (MHC class I-related molecule) is a protein found in every cell of the human body that functions as a molecular alarm system, alerting powerful cells of our immune system, our white blood cells, when cancer or bacterial infection is present.
While prior groundbreaking research revealed the cellular machinery that MR1 depends on to activate, nothing was understood about how the MR1 alarm is “turned off” until now.