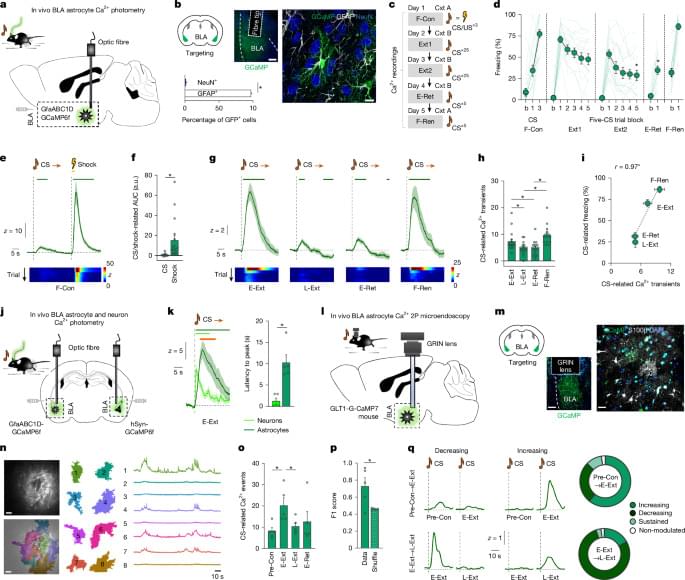
A thorough study exploring how astrocytes affect fear conditioning and fear extinction in the basolateral amygdala of mice. Subpopulations of astrocytes were found to interact with neurons in such a way as to help encode representations of fear. [ https://www.nature.com/articles/s41586-025-10068-0](https://www.nature.com/articles/s41586-025-10068-0)
Gq G-protein-coupled receptor (GPCR) signalling increases astrocyte Ca2+ activity through IP3-mediated release of intracellular Ca2+ stores42,43 and hM3Dq actuation causes a Ca2+ surge preceded by prolonged quiescence, possibly due to intracellular Ca2+ depletion24,44,45. Replicating these effects in the BLA, we expressed hM3Dq in BLA astrocytes and used in vivo cyto-GCaMP6f photometry and observed that clozapine–N-oxide (CNO) injection markedly increased Ca2+ activity within around 10 min but, thereafter, decreased and remained low for at least 2 h (Fig. 2c and Extended Data Figs. 6a–e and 8e, f). A lower hM3Dq virus concentration or lower CNO dose had modest or negligible effects on Ca2+ activity and behaviour (Extended Data Fig. 6h–p). On the basis of these data, we posited that BLA astrocyte Ca2+ dynamics would be constrained by hM3Dq actuation at timepoints relevant to behavioural testing. Consistent with this supposition, hM3Dq-actuation essentially abolished Ca2+ responses to a potent stimulus (footshock) given 30 min after CNO injection (Extended Data Fig. 6f, g).
We leveraged these effects of hM3Dq actuation to test how constraining astrocyte Ca2+ dynamics affected memory acquisition, retrieval, consolidation and extinction by injecting separate groups of animals with 3 mg per kg CNO either before or immediately after F-Con, or before fear retrieval/extinction training. We found that CNO given before extinction training reduced CS-related freezing during E-Ext—consistent with impaired memory retrieval—in hM3Dq-expressing mice compared with viral controls (Fig. 2d, e). In vivo fibre photometry confirmed that this behavioural effect was accompanied by loss of CS-related astrocyte Ca2+ responses (Fig. 2f and Extended Data Fig. 7a–c). In contrast to these memory-retrieval-impairing effects, CNO had no behavioural effect when injected before or after F-Con26,27 and did not alter uncued freezing, shock-induced flinching or various measures of anxiety-like behaviour (Extended Data Fig. 7d–i). Behavioural effects were also absent when CNO was injected in mice not expressing hM3Dq or when vehicle was injected in hM3Dq-expressing animals, excluding potential non-specific CNO and hM3Dq-virus effects, respectively (Extended Data Fig. 7j–n).
We next compared these effects with those of another DREADD, hM4Di, that produces effects on cortical, striatal and (as we show here; Fig. 2g–i) BLA astrocyte Ca2+ activity that mirror those of hM3Dq, that is, increase Ca2+ transients24,46,47. Accordingly, we found that hM4Di actuation produced effects on memory retrieval that were opposite to hM3Dq: pre-Ext CNO injection produced increases in CS-related freezing and astrocyte Ca2+ responses during E-Ext in hM4Di-expressing mice compared with viral controls (Fig. 2j–l and Extended Data Fig. 8a–f). Pre-Ext hM4Di actuation also increased freezing during (CNO-free) E-Ret, indicative of a deficit in extinction memory formation, and attenuated CS-related Ca2+ activity during this test stage. This latter effect is notable given that hM3Dq actuation produced a similar extinction deficit and blunted the CS-related Ca2+ response on E-Ret (Fig. 2e and Extended Data Fig. 7b), despite the two manipulations having opposite effects on fear retrieval and neither affecting extinction memory when CNO was given before E-Ret (Extended Data Fig. 8g, h). This convergence of extinction-impairing effects suggests that extinction is sensitive to perturbations—whether increases or decreases—in astrocyte Ca2+ activity and, by extension, implies an important role for BLA astrocytes in the plastic adaptations underlying extinction memory formation.