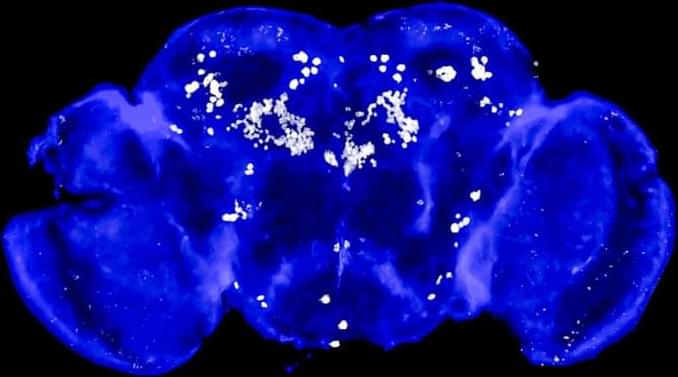
Aging, the key risk factor for cognitive decline, impacts the brain in a region-specific manner, with microglia among the most affected cell types. However, it remains unclear whether this is intrinsically mediated or driven by age-related changes in neighboring cells. Here, we describe a scalable, genetically modifiable system for in vivo heterochronic myeloid cell replacement. We find reconstituted myeloid cells adopt region-specific transcriptional, morphological and tiling profiles characteristic of resident microglia. Young donor cells in aged brains rapidly acquired aging phenotypes, particularly in the cerebellum, while old cells in young brains adopted youthful profiles. We identified STAT1-mediated signaling as one axis controlling microglia aging, as STAT1-loss prevented aging trajectories in reconstituted cells. Spatial transcriptomics combined with cell ablation models identified rare natural killer cells as necessary drivers of interferon signaling in aged microglia. These findings establish the local environment, rather than cell-autonomous programming, as a primary driver of microglia aging phenotypes.
Claire Gizowski, Galina Popova, Heather Shin, Wendy Craft, Wenjun Kong, Bernd J Wranik, Yuheng C Fu, Tzuhua D Lin, Baby Martin-McNulty, Po-Han Tai, Kayla Leung, Nicole Fong, Devyani Jogran, Agnieszka Wendorff, David Hendrickson, Astrid Gillich, Andy Chang, Oliver Hahn are current or former employees of Calico Life Sciences LLC. The remaining authors declare no competing interest.