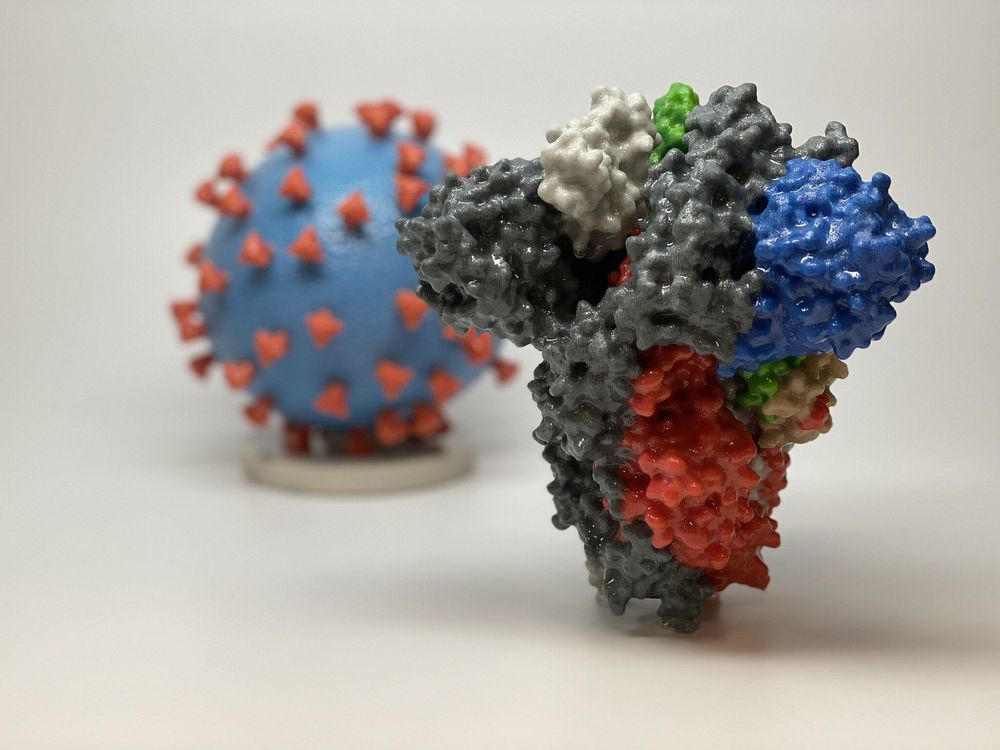
“These findings reveal how the immune system goes awry during coronavirus infections, leading to severe disease, and point to potential therapeutic targets,” said Bali Pulendran, Ph.D., professor of pathology and of microbiology and immunology and the senior author of the study, which will be published Aug. 11 in Science.
Lead authorship is shared by Stanford postdoctoral scholars Prabhu Arnunachalam, Ph.D., and Florian Wimmers, Ph.D.; and Chris Ka Pun Mok, Ph.D., and Mahen Perera, Ph.D., both assistant professors of public health laboratory sciences at the University of Hong Kong.
A Stanford study shows that in severely ill COVID-19 patients, “first-responder” immune cells, which should react immediately to signs of viruses or bacteria in the body, instead respond sluggishly.
Some people get really sick from COVID-19, and others don’t. Nobody knows why.
Now, a study by investigators at the Stanford University of Medicine and other institutions has turned up immunological deviations and lapses that appear to spell the difference between severe and mild cases of COVID-19.