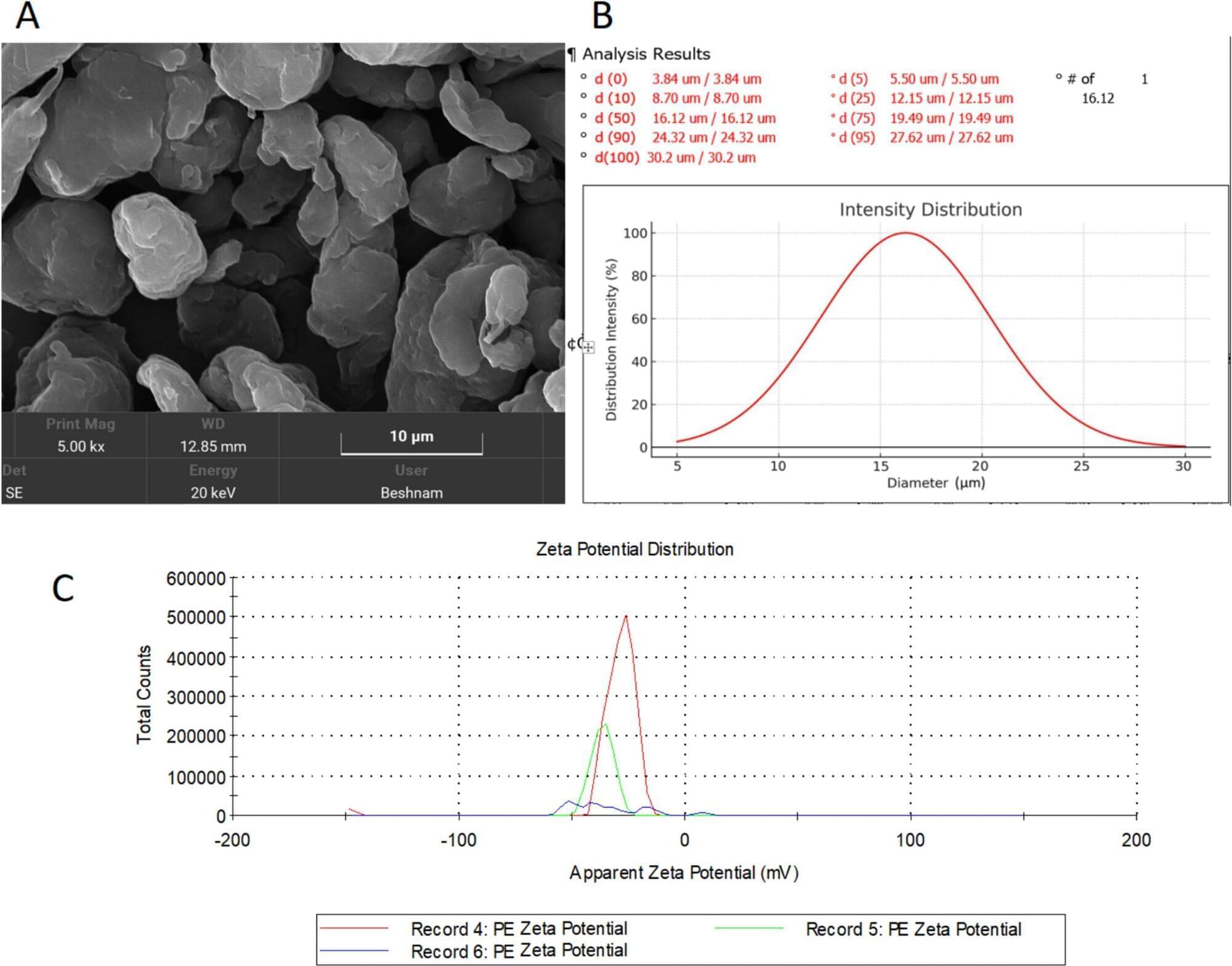
The widespread prevalence of plastics and in particular, microplastics (MPs) raises concerns about their potential toxic effects. MPs, defined as particles smaller than 5 mm, are distributed throughout ecosystem and can enter the human body through the food chain. There is a lack of knowledge regarding MP potential harmful effects on the mammal’s body, especially the brain. This study aimed to examine the impact of low-density polyethylene (LDPE) MPs (< 30 μm) on blood–brain barrier (BBB) integrity, oxidative stress, and neuronal health. Male rats were exposed to LDPE MPs via oral administration for 3 and 6 weeks. The results revealed no significant changes in brain water content across groups. However, BBB integrity was significantly compromised after both 3 and 6 weeks of exposure. Oxidative stress increased in MP-treated groups, evidenced by decreased superoxide dismutase (SOD) levels and elevated malondialdehyde (MDA). Additionally, brain-derived neurotrophic factor (BDNF) levels significantly declined in the 6-week group. Histological analysis indicated neuronal damage and death in both treatment durations. These findings demonstrate that chronic exposure to LDPE MPs impairs BBB integrity, increases oxidative stress, and induces neuronal damage in rats. The results highlight the neurotoxic potential of MPs and emphasize the need for further research to address their possible health risks.