Hibernation Biology & Applications In Human Health & Resilience — Dr. Dana K. Merriman, Ph.D., Distinguished Professor Emerita of Biology; Director of the Squirrel Colony, UW-Oshkosh.
Dr. Dana K. Merriman Ph.D. (www.uwosh.edu/facstaff/merriman/VaughanHome), is Distinguished Professor Emerita of Biology, and Director of the Squirrel Colony, at University of Wisconsin Oshkosh, and Adjunct Professor of Ophthalmology & Visual Sciences, Medical College of Wisconsin.
With her BA in Biological Science and her PhD in Physiology and Cell Biology, both from University of California-Santa Barbara, as well as having spent time as a Postdoctoral Fellow at University of Utah Health Sciences Center, a core focus of Dr. Merriman’s laboratory research over the years has been the development of a captive breeding colony of the 13-lined ground squirrels.
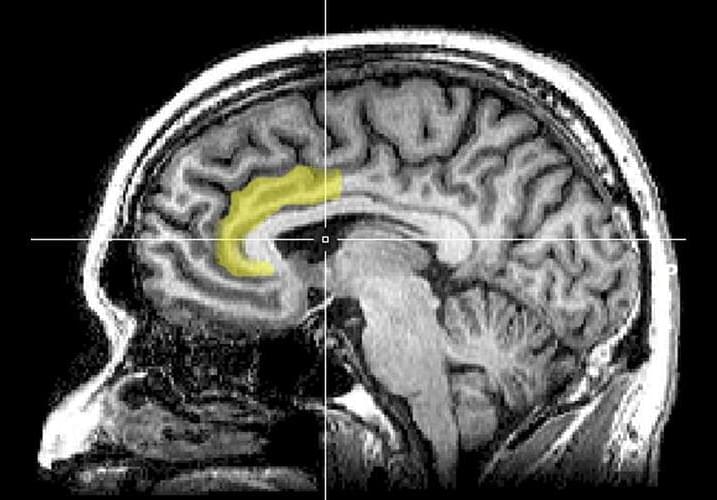
This unique, one-of-a-kind captive breeding program, due to this species very unique cone-dominant, diurnal visual system, as well as their impressive physiological ability to survive in hibernation for over six months without food or water, has served investigators with animals and custom-dissected tissues from the US, Asia, and Europe for decades, as well as been core to Dr Merriman’s own work on vision, including cone cell biology and retinal function during the metabolic state transitions associated with hibernation.
Over the years, Dr. Merriman expanded her research horizon well outside of vision, into neuroscience, and in recent years she has collaborated on studies of muscle physiology, viral genomics, molecular biology of transposable elements, and comparative genetics of the control of coat patterning.